CNN —
A panel of independent experts that advises the US Food and Drug Administration on its vaccine decisions voted unanimously Thursday to update all Covid-19 vaccines so they contain the same ingredients as the two-strain shots that are now used as booster doses.
The vote means young children and others who haven’t been vaccinated may soon be eligible to receive two-strain vaccines that more closely match the circulating viruses as their primary series.
The FDA must sign off on the committee’s recommendation, which it is likely to do, before it goes into effect.
Currently, the US offers two types of Covid-19 vaccines. The first shots people get – also called the primary series – contain a single set of instructions that teach the immune system to fight off the original version of the virus, which emerged in 2019.
This index strain is no longer circulating. It was overrun months ago by an ever-evolving parade of new variants.
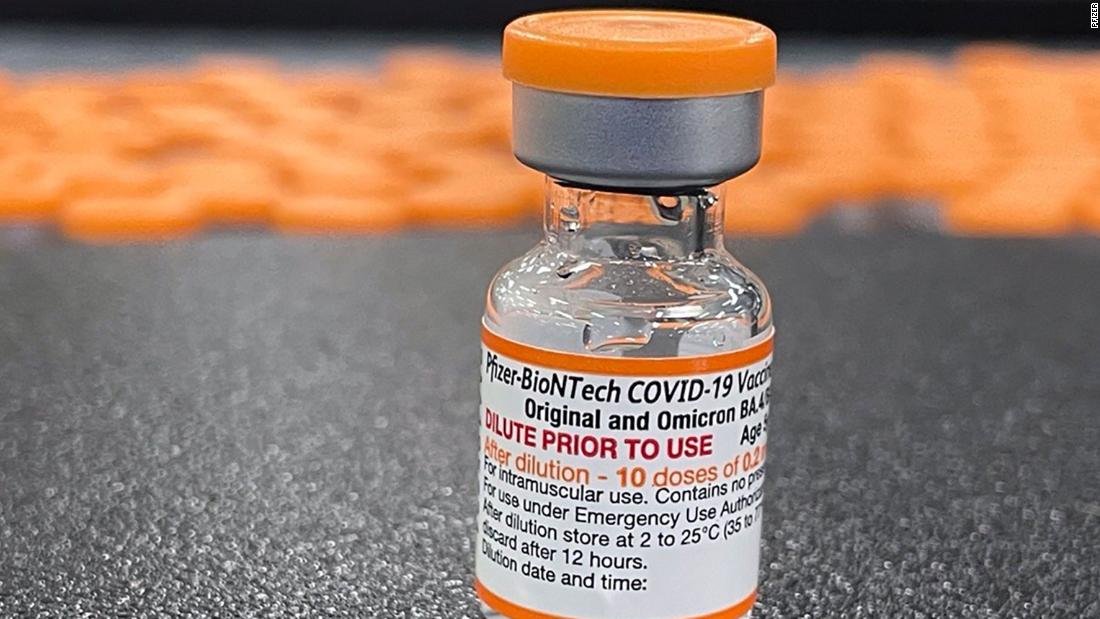
Last year, in consultation with its advisers, the FDA decided that it was time to update the vaccines. These two-strain, or bivalent, shots contain two sets of instructions; one set reminds the immune system about the original version of the coronavirus, and the second set teaches the immune system to recognize and fight off Omicron’s BA.4 and BA.5 subvariants, which emerged in the US last year.
People who have had their primary series – nearly 70% of all Americans – were advised to get the new two-strain booster late last year in an effort to upgrade their protection against the latest variants.
The advisory committee heard testimony and data suggesting that the complexity of having two types of Covid-19 vaccines and schedules for different age groups may be one of the reasons for low vaccine uptake in the US.
Currently, only about two-thirds of Americans have had the full primary series of shots. Only 15% of the population has gotten an updated bivalent booster.
Data presented to the committee shows that Covid-19 hospitalizations have been rising for children under the age of 2 over the past year, as Omicron and its many subvariants have circulated. Only 5% of this age group, which is eligible for Covid-19 vaccination at 6 months of age, has been fully vaccinated. Ninety percent of children under the age of 4 are still unvaccinated.
“The most concerning data point that I saw this whole day was that extremely low vaccination coverage in 6 months to 2 years of age and also 2 years to 4 years of age,” said Dr. Amanda Cohn, director of the US Centers for Disease Control and Prevention’s Division of Birth Defects and Infant Disorders. “We have to do much, much better.”
Cohn says that having a single vaccine against Covid-19 in the US for both primary and booster doses would go a long way toward making the process less complicated and would help get more children vaccinated.
Others feel that convenience is important but also stressed that data supported the switch.
“This isn’t only a convenience thing, to increase the number of people who are vaccinated, which I agree with my colleagues is extremely important for all the evidence that was related, but I also think moving towards the strains that are circulating is very important, so I would also say the science supports this move,” said Dr. Hayley Gans, a pediatric infectious disease specialist at Stanford University.
Many others on the committee were similarly satisfied after seeing new data on the vaccine effectiveness of the bivalent boosters, which are cutting the risk of getting sick, being hospitalized or dying from a Covid-19 infection.
“I’m totally convinced that the bivalent vaccine is beneficial as a primary series and as a booster series. Furthermore, the updated vaccine safety data are really encouraging so far,” said Dr. David Kim, director of the the US Department of Health and Human Services’ National Vaccine Program, in public discussion after the vote.
Thursday’s vote is part of a larger plan by the FDA to simplify and improve the way Covid-19 vaccines are given in the US.
The agency has proposed a plan to convene its vaccine advisers – called the Vaccines and Related Biological Products Advisory Committee, or VRBPAC – each year in May or June to assess whether the instructions in the Covid-19 vaccines should be changed to more closely match circulating strains of the virus.
The time frame was chosen to give manufacturers about three months to redesign their shots and get new doses to pharmacies in time for fall.
“The object, of course – before anyone says anything – is not to chase variants. None of us think that’s realistic,” said Jerry Weir, director of the Division of Viral Products in the FDA’s Office of Vaccines Research and Review.
“But I think our experience so far, with the bivalent vaccines that we have, does indicate that we can continue to make improvements to the vaccine, and that would be the goal of these meetings,” Weir said.
In discussions after the vote, committee members were supportive of this plan but pointed out many of the things we still don’t understand about Covid-19 and vaccination that are likely to complicate the task of updating the vaccines.
For example, we now seem to have Covid-19 surges in the summer as well as the winter, noted Dr. Michael Nelson, an allergist and immunologist at the University of Virginia. Are the surges related? And if so, is fall the best time to being a vaccination campaign?
The CDC’s Dr. Jefferson Jones said that with only three years of experience with the virus, it’s really too early to understand its seasonality.
Other important questions related to the durability of the mRNA vaccines and whether other platforms might offer longer protection.
“We can’t keep doing what we’re doing,” said Dr. Bruce Gellin, chief of global public health strategy at the Rockefeller Foundation. “It’s been articulated in every one of these meetings despite how good these vaccines are. We need better vaccines.”
The committee also encouraged both government and industry scientists to provide a fuller picture of how vaccination and infection affect immunity.
One of the main ways researchers measure the effectiveness of the vaccines is by looking at how much they increase front-line defenders called neutralizing antibodies.
Neutralizing antibodies are like firefighters that rush to the scene of an infection to contain it and put it out. They’re great in a crisis, but they tend to diminish in numbers over time if they’re not needed. Other components of the immune system like B-cells and T-cells hang on to the memory of a virus and stand ready to respond if the body encounters it again.
Scientists don’t understand much about how well Covid-19 vaccination boosts these responses and how long that protection lasts.
Another puzzle will be how to pick the strains that are in the vaccines.
The process of selecting strains for influenza vaccines is a global effort that relies on surveillance data from other countries. This works because influenza strains tend to become dominant and sweep around the world. But Covid-19 strains haven’t worked in quite the same way. Some that have driven large waves in other countries have barely made it into the US variant mix.
“Going forward, it is still challenging. Variants don’t sweep across the world quite as uniform, like they seem to with influenza,” the FDA’s Weir said. “But our primary responsibility is what’s best for the US market, and that’s where our focus will be.”
Eventually, the FDA hopes that Americans would be able to get an updated Covid-19 shot once a year, the same way they do for the flu. People who are unlikely to have an adequate response to a single dose of the vaccine – such as the elderly or those with a weakened immune system – may need more doses, as would people who are getting Covid-19 vaccines for the first time.
At Thursday’s meeting, the advisory committee also heard more about a safety signal flagged by a government surveillance system called the Vaccine Safety Datalink.
The CDC and the FDA reported January 13 that this system, which relies on health records from a network of large hospital systems in the US, had detected a potential safety issue with Pfizer’s bivalent boosters.
In this database, people 65 and older who got a Pfizer bivalent booster were slightly more likely to have a stroke caused by a blood clot within three weeks of their vaccination than people who had gotten a bivalent booster but were 22 to 42 days after their shot.
After a thorough review of other vaccine safety data in the US and in other countries that use Pfizer bivalent boosters, the agencies concluded that the stroke risk was probably a statistical fluke and said no changes to vaccination schedules were recommended.
At Thursday’s meeting, Dr. Nicola Klein, a senior research scientist with Kaiser Permanente of Northern California, explained how they found the signal.
The researchers compared people who’d gotten a vaccine within the past three weeks against people who were 22 to 42 days away from their shots because this helps eliminate bias in the data.
When they looked to see how many people had strokes around the time of their vaccination, they found an imbalance in the data.
Of 550,000 people over 65 who’d received a Pfizer bivalent booster, 130 had a stroke caused by a blood clot within three weeks of vaccination, compared with 92 people in the group farther out from their shots.
The researchers spotted the signal the week of November 27, and it continued for about seven weeks. The signal has diminished over time, falling from an almost two-fold risk in November to a 47% risk in early January, Klein said. In the past few days, it hasn’t been showing up at all.
Klein said they didn’t see the signal in any of the other age groups or with the group that got Moderna boosters. They also didn’t see a difference when they compared Pfizer-boosted seniors with those who were eligible for a bivalent booster but hadn’t gotten one.
Further analyses have suggested that the signal might be happening not because people who are within three weeks of a Pfizer booster are having more strokes, but because people who are within 22 to 42 days of their Pfizer boosters are actually having fewer strokes.
Overall, Klein said, they were seeing fewer strokes than expected in this population over that period of time, suggesting a statistical fluke.
Another interesting thing that popped out of this data, however, was a possible association between strokes and high-dose flu vaccination. Seniors who got both shots on the same day and were within three weeks of those shots had twice the rate of stroke compared with those who were 22 to 42 days away from their shots.
What’s more, Klein said, the researchers didn’t see the same association between stroke and time since vaccination in people who didn’t get their flu vaccine on the same day.
The total number of strokes in the population of people who got flu shots and Covid-19 boosters on the same day is small, however, which makes the association a shaky one.
“I don’t think that the evidence are sufficient to conclude that there’s an association there,” said Dr. Tom Shimabukuro, director of the CDC’s Immunization Safety Office.
Nonetheless, Richard Forshee, deputy director of the FDA’s Office of Biostatistics and Pharmacovigilance, said the FDA is planning to look at these safety questions further using data collected by Medicare.
The FDA confirmed that the agency is taking a closer look.
“The purpose of the study is 1) to evaluate the preliminary ischemic stroke signal reported by CDC using an independent data set and more robust epidemiological methods; and 2) to evaluate whether there is an elevated risk of ischemic stroke with the COVID-19 bivalent vaccine if it is given on the same day as a high-dose or adjuvanted seasonal influenza vaccine,” a spokesperson said in a statement.
The FDA did not give a time frame for when these studies might have results.